Changes to Medicare in the Inflation Reduction Act
The Inflation Reduction Act of 2022 has transformed Medicare, mainly in the way Medicare pays for medications. These changes will affect patients that get their drug coverage through Medicare, including beneficiaries with Part D plans and Medicare Advantage plans. If they offer drug coverage, Medicare HMO plans are also included in these changes.
Medicare Part D Changes and the New Medicare Prescription Payment Plan
Medicare prescription drug coverage, known as Part D, is undergoing major changes. With the updated benefit design, you won't have to deal with multiple coverage phases for your prescription costs any longer, and the coverage gap is gone. Instead, you'll pay for your prescriptions (after paying a deductible, if applicable) until you reach your annual out-of-pocket limit of $2,000. In addition, there is a new Medicare Prescription Payment Plan that could change how you pay for your medications.
Medicare prescription drug coverage, known as Part D, is undergoing major changes. With the updated benefit design, you won't have to deal with multiple coverage phases for your prescription costs any longer, and the coverage gap is gone. Instead, you'll pay for your prescriptions (after paying a deductible, if applicable) until you reach your annual out-of-pocket limit of $2,000. In addition, there is a new Medicare Prescription Payment Plan that could change how you pay for your medications.
What is it?
The Medicare Prescription Payment Plan allows people with Medicare prescription coverage (Part D) to pay their out-of-pocket prescription drug costs in monthly installments instead of all at once. You are not automatically enrolled in the program; you must choose to opt in. Anyone with a Part D plan can opt into the program at any time during the year. The Medicare Prescription Payment Plan only applies to Part D and Medicare Advantage plans that offer Part D benefits.
How does it work?
If you opt-in to the program, you will not pay for medications at the pharmacy when you pick up your prescription. Instead, your Part D plan will pay the pharmacy, and your plan will send you bills for the amount you owe during each of the remaining months of the year. This is referred to as “smoothing” and is a way to spread your out-of-pocket medication costs out over the year, paying part of the costs each month up to the maximum amount of $2000 in total for the year.
Does this save me money?
This program doesn’t lower your out-of-pocket costs for prescriptions. However, it may make paying for medications more manageable by spreading the costs throughout the year instead of all at once.
How do you sign up?
During the 2025 Open Enrollment period, individuals with Part D or Medicare Advantage plans that cover prescriptions can enroll in the Medicare Prescription Payment Plan. Contact your Part D plan provider and follow the enrollment process to enroll. You or your authorized representative can submit an election request to join the program. You can submit this request by paper, phone, or online. Your Part D plan will process your enrollment request within 24 hours.
What medications are included in the Medicare Prescription Payment Plan?
All Medicare Part D drugs are included in the program. Part D plans cannot exclude any covered medications. Once you opt into the Medicare Prescription Payment Plan, all your out-of-pocket prescription drug costs will be billed monthly as required, as long as you remain in the plan.
What happens if I don’t pay? Do I lose my insurance?
If you don’t pay the amount your Part D plan bills you, your participation in the program may be terminated and any amount you owe your plan will become due immediately. However, you will not lose your Part D coverage. Your insurance company cannot send you to collections if you have outstanding amounts due for prescription medication costs and they cannot charge you any fees on the balance. You will not be allowed to participate in the prescription payment plan in the future until you pay all outstanding balances that you owe to your Part D plan.
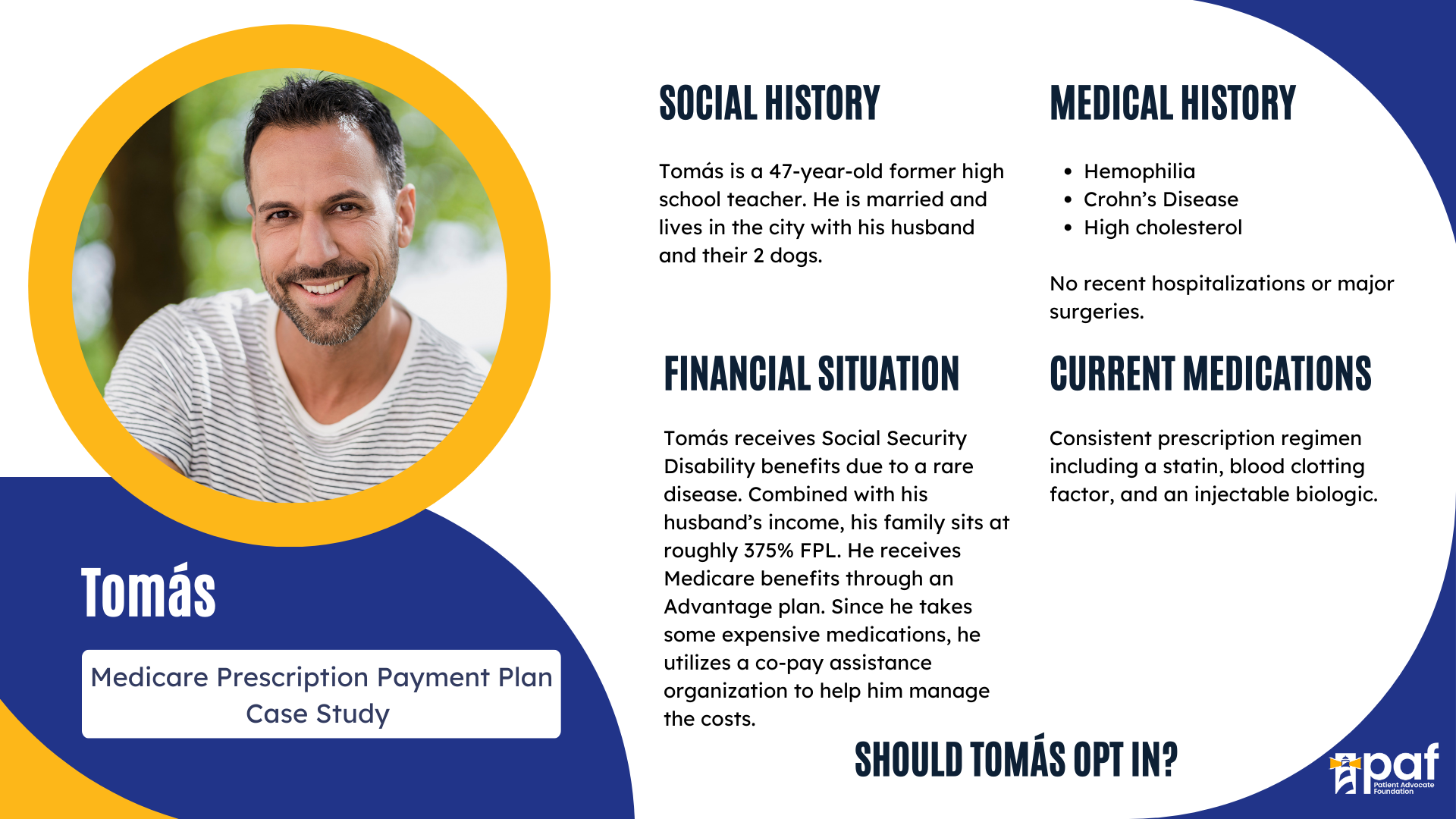
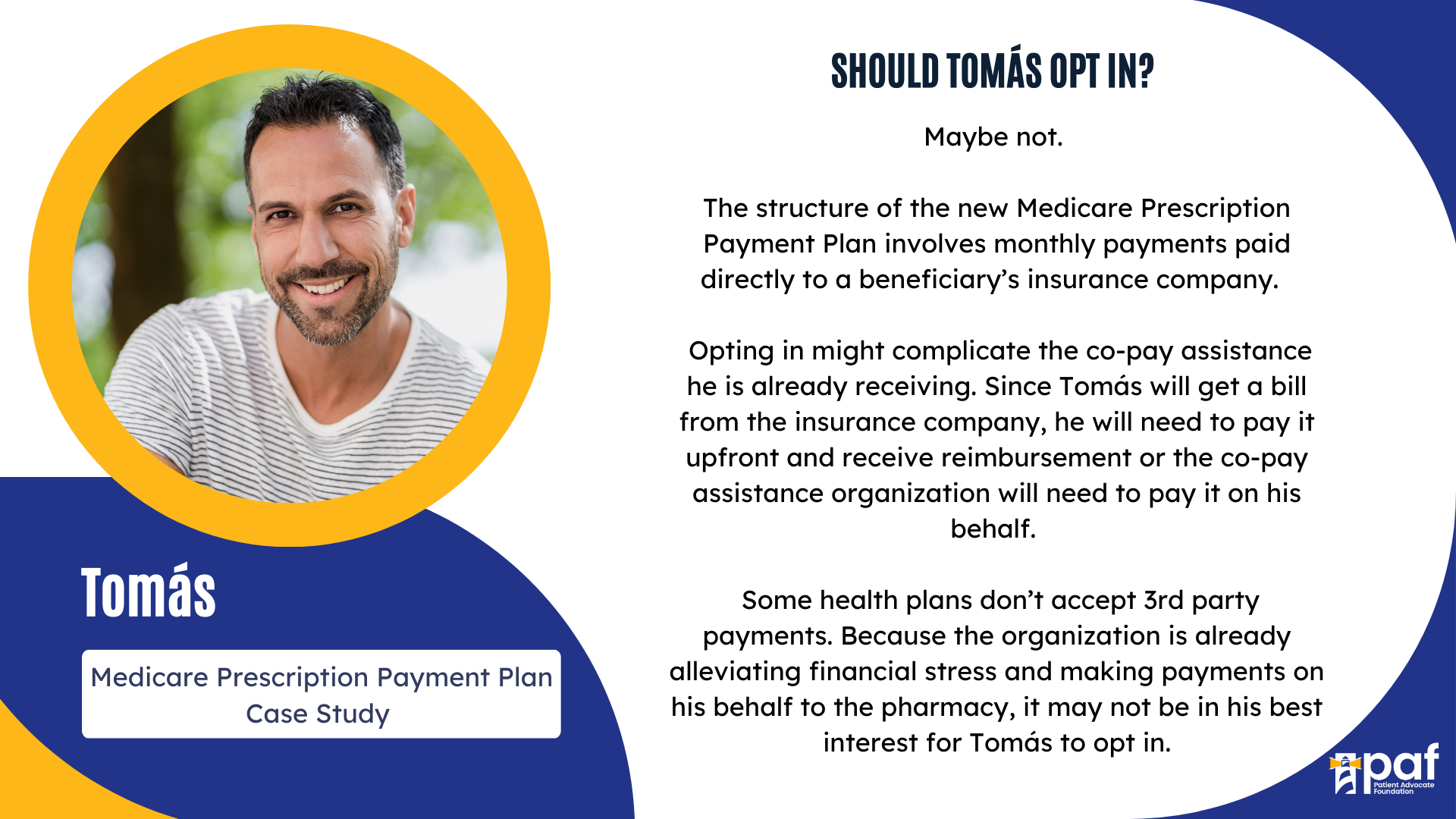
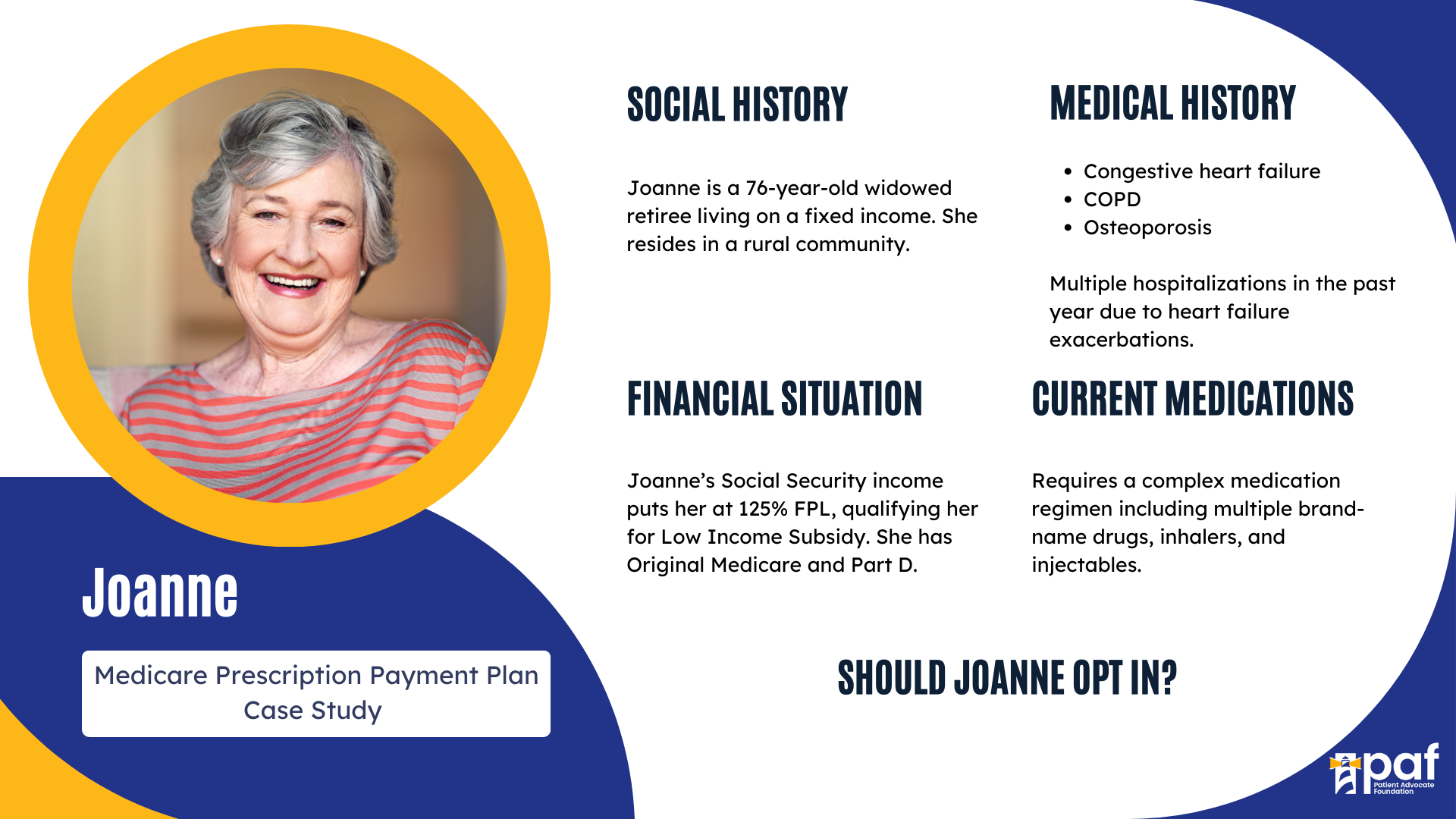
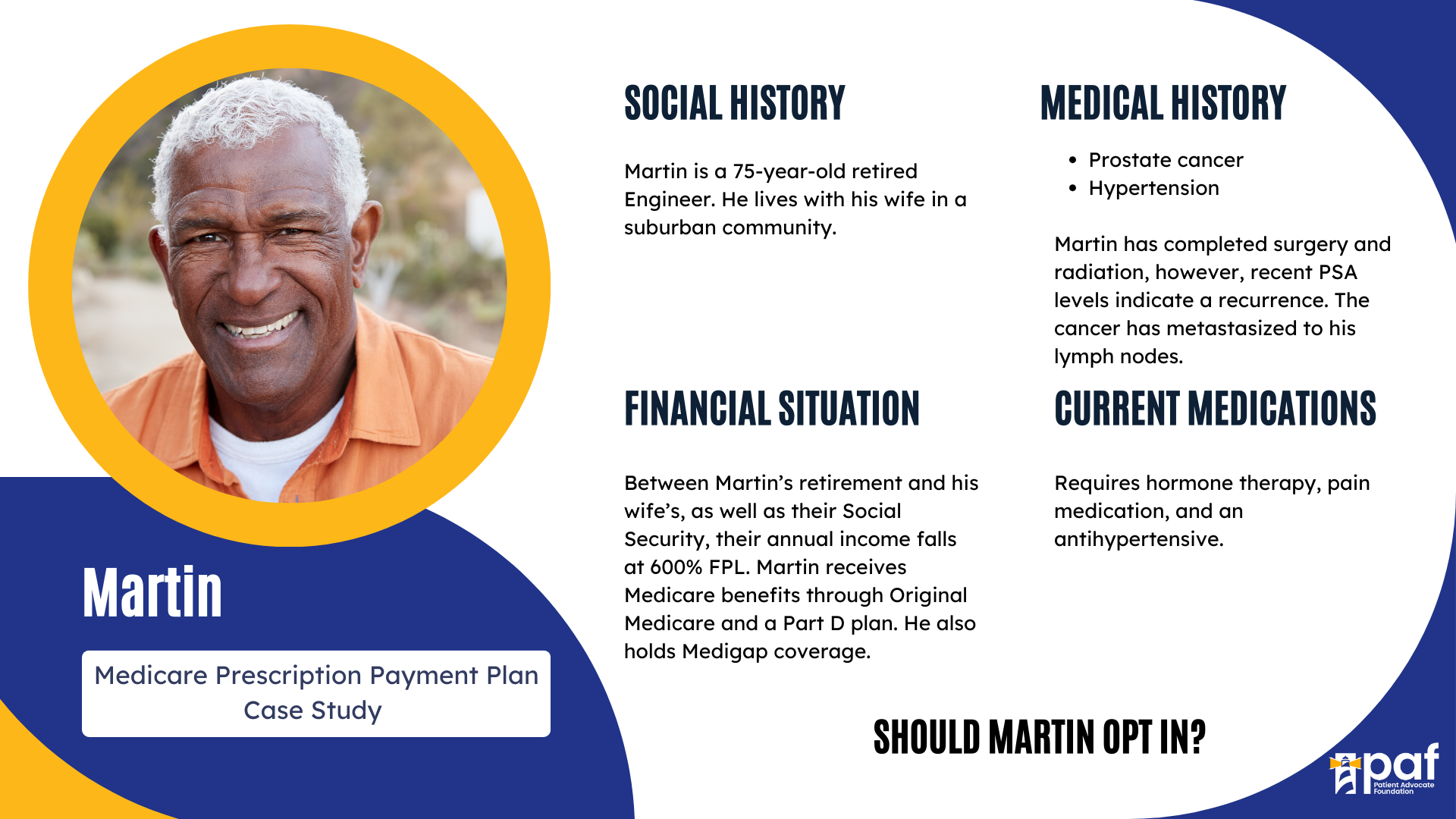
How do I know if I am a good fit for the program?
- People with high prescription medication costs that cause them to hit the $2,000 out-of-pocket cap earlier in the year may benefit from this program.
- If you receive assistance from a charitable foundation for some or all of your medication costs, you may not benefit from this program.
- It is important to determine what is best for you based on your annual medication costs and any help you may receive from a third-party organization before enrolling as the payment plan may, or may not, be the best fit for you.
How can I make the most of the Prescription Payment Plan?
- Make sure you understand what you are paying. You can always contact your Part D plan or the pharmacy to ensure you understand your costs.
- Making sure that you are keeping up with payments. If the program works for you, it’s best to ensure you pay your bills on time to remain on the Payment Plan.
- Make sure you communicate with your insurance company in case there are shifts or changes with the prescription payment plan.
Key Dates:
October 15, 2024: Medicare Open Enrollment begins. You can now opt into the Medicare Prescription Payment Plan for the 2025 plan year.
December 7, 2024: Medicare Open Enrollment Ends.
January 1, 2025: The Medicare Prescription Payment Plan launches.
January 1, 2025-December 31, 2025: Part D enrollees can opt into the payment plan at any time throughout the year.
It is important to carefully consider your situation and the specific details of the program before deciding if opting into the Medicare Prescription Payment Plan is right for you.
How can you learn more?
The Centers for Medicare and Medicaid Services (CMS) will create various educational resources for Part D enrollees, pharmacies, prescribers, and others. These materials will be available before the 2025 Medicare Open Enrollment Period. You will also hear additional information on opting in from your Part D plan.How the Inflation Reduction Act Impacts Medicare
Out-of-pocket expenses capped
Currently, seniors who exceed the catastrophic coverage amount of $7,050 are stuck with a 5% coinsurance fee. In 2024, that fee will be eliminated, resulting in a savings of about $2,700 per year for about a million patients. This change will reduce the out-of-pocket maximum to approximately $3,250.
Starting in 2025, out-of-pocket costs for medications will be capped at $2000.
Insulin costs $35
Starting immediately, out-of-pocket costs for insulin are capped at $35 per month.
Vaccines are free.
All of them, right now, including COVID.
Extended subsidies for low-income seniors
Starting in 2024, seniors whose incomes are at or below 150% FPL (in 2023, $1699 per month) will have no Part D premiums or deductibles. They will not be responsible for any copays after they reach the catastrophic threshold.
Medicare Can Negotiate [Some] Drug Prices
When Congress created Medicare Part D, the prescription drug plan, it specifically prohibited Medicare from negotiating drug prices with drug companies. The individual Medicare Part D plans, bought by seniors through Humana, Blue Cross Blue Shield, United, etc, could negotiate but not Medicare as a whole entity.
In 2026, Medicare can begin negotiating prices for 10 of the highest-spending Medicare-covered drugs. In 2027, Medicare will add 15 more drugs, another 15 in 2028 and finally 20 more in 2029. The Centers for Medicare and Medicaid Services (CMS) has until September 2023 to select the drugs.
Current and Future Changes
2025
☐ People with Medicare Part D won’t pay more than $2,000 out-of-pocket for prescription drugs per year. This only applies to drugs covered by your prescription drug plan.
☐ People with Medicare Part D have the option to pay the $2,000 out-of-pocket prescription drug costs in monthly installments (also called “smoothing’). To learn more, click here
☐ The Manufacturer Discount Program will require manufacturer discounts for applicable drugs in the initial coverage and catastrophic phases.
☐ Government reinsurance in the catastrophic phase of Part D will decrease from 80% to 20% for brand-name drugs, biologicals, and biosimilars and will decrease from 80% to 40% for generics.
☐ By Feb 1, CMS announces 15 more Part D drugs in the Drug Price Negotiation Program. By Nov 30, CMS publishes the maximum fair prices for those additional 15 drugs and prices go into effect in 2027.
2026
☐ Maximum fair prices for the first 10 Medicare Part D drugs in the Drug Price Negotiation Program go into effect. (This is the first year people with Medicare will benefit from the Drug Price Negotiation Program.) By Feb 1, CMS will announce 15 new drugs and maximum fair prices will be announced by Nov 30. Maximum fair prices go into effect in 2028.
☐ Government reinsurance in the catastrophic phase of Part D will be 40% for Medicare Part D drugs selected for negotiation in their applicability period.
2027 - 2029
☐ Additional drugs are selected for the Drug Price Negotiation Program, and maximum fair prices for new drugs are phased in each year.
Changes Already Implemented
2023
☐ Insulin co-pays are limited to $35/month and Part D deductibles won’t apply to covered insulin products. Learn more about Insulin Coverage (medicare.gov)
☐ Vaccines recommended by the Advisory Committee on Immunization Practices (ACIP) are available at no cost.
☐ Lower coinsurance for Part B drugs if the drug price increased faster than inflation.
☐ By Sept 1, CMS announces the first 10 Part D drugs selected for the Drug Price Negotiation Program (which establishes maximum fair drug prices). Click here to see a detailed list of 2023 Medicare changes
2024
☐ Elimination of the 5% coinsurance for Part D catastrophic coverage, which will cap out-of-pocket costs at approximately $3250.
☐ Part D premiums will not exceed a 6% increase each year (2024-2030).
☐ The federal Low-Income Subsidy (LIS) or Extra Help Program will be available to people who earn less than 150% of the federal poverty level. With full benefits, most out-of-pocket costs for prescription drugs will be covered.
☐ There will be a cap on Part B payment for new biosimilars.
☐ By Sept 1, CMS publishes the maximum fair prices of the first 10 drugs in the Drug Price Negotiation Program, and prices go into effect in 2026.

The Inflation Reduction Act of 2022 affects everyone on Medicare. See what changes are coming your way as a Medicare beneficiary in 2023 and beyond.

Explore informational and cost-saving resources for Medicare beneficiaries from state and national sources.